How I Learned to Dance with the Heavy Days: My Real Journey Through Depression Adjustment
Depression doesn’t announce itself with sirens—more like a slow fog creeping into your mornings, making everything feel heavier. I didn’t realize I was slipping until simple tasks felt impossible. But over time, I discovered small, science-backed shifts that didn’t promise miracles but offered real relief. This is not a cure story. It’s about learning to adjust, prevent relapses, and reclaim daily life—one honest step at a time.
The Quiet Descent: Recognizing the Early Signs of Emotional Shifts
Depression often begins quietly, masked as fatigue, irritability, or disinterest. Unlike grief or sadness, which are reactions to specific events, depression lingers without clear cause, shaping how a person sees themselves and the world. Many women between 30 and 55 report that their first awareness of emotional decline came not from dramatic breakdowns, but from noticing they no longer enjoyed activities they once loved—reading, gardening, spending time with children. These shifts can be so gradual that they blend into daily life, dismissed as stress or aging.
Scientific research confirms that early recognition of depressive symptoms significantly improves long-term outcomes. According to the National Institute of Mental Health, persistent low mood, changes in sleep or appetite, difficulty concentrating, and feelings of worthlessness lasting more than two weeks may indicate clinical depression. Yet many wait months—or years—before seeking support, often because the symptoms don’t feel “serious enough.” This delay allows patterns of negative thinking and physical lethargy to deepen, making recovery more complex.
Understanding personal triggers is essential. For some, hormonal changes during perimenopause contribute to mood fluctuations. For others, caregiving responsibilities, financial stress, or chronic illness create emotional strain. Keeping a mood journal, even informally, helps identify patterns—such as increased fatigue on rainy days or low mood after certain social interactions. Awareness doesn’t require diagnosis; it simply means paying attention. When you begin to notice the fog before it thickens, you gain the power to respond earlier, with gentler tools.
Early intervention isn’t about fixing everything at once. It’s about acknowledging that something has shifted and allowing space to respond with care. Small actions—like stepping outside for five minutes of sunlight or calling a trusted friend—can interrupt the downward spiral. The goal isn’t to eliminate difficult emotions but to prevent them from becoming entrenched. By treating emotional health with the same attentiveness as physical health, women can build resilience before symptoms escalate.
Mind Over Myth: Rewriting the Story of Depression
One of the most painful aspects of depression isn’t the sadness itself, but the shame that surrounds it. Misconceptions persist: that depression is a sign of personal weakness, a lack of gratitude, or simply a phase that will pass if one tries harder. These myths do more than misinform—they isolate. When women believe they should be able to “snap out of it,” they may hide their struggles, fearing judgment or failure. This silence deepens the emotional burden, making recovery harder.
Modern neuroscience shows that depression is not a character flaw but a complex interplay of biology, psychology, and environment. Brain imaging studies reveal differences in activity within regions responsible for mood regulation, decision-making, and self-perception. Chemical imbalances involving serotonin, norepinephrine, and dopamine are well-documented contributors, though not the sole cause. Genetics, chronic stress, inflammation, and early life experiences all shape vulnerability. Understanding this helps reframe depression not as a failure, but as a condition that responds to care and support.
Cognitive psychology further explains how thought patterns reinforce depressive states. Negative self-talk—“I’m not good enough,” “Nothing will ever change”—becomes automatic over time, shaping perception and behavior. These loops aren’t lies, but distortions shaped by emotional pain. The good news is that cognitive restructuring, a technique used in cognitive behavioral therapy (CBT), can help identify and gently challenge these patterns. It doesn’t erase pain but creates space to respond differently.
Adjusting to life with depression isn’t about achieving constant happiness. It’s about learning new ways to relate to your mind. Just as you wouldn’t blame yourself for needing glasses to see clearly, you don’t need to blame yourself for needing support to feel steady. Normalizing mental health care—whether through therapy, lifestyle changes, or medication—removes stigma and opens doors to healing. When we stop seeing depression as a moral failing and start seeing it as a signal for care, recovery becomes possible.
The Body-Mind Connection: Movement as Gentle Rebellion
When energy is low and motivation feels out of reach, the idea of exercise can seem impossible, even insulting. Yet movement—gentle, consistent, and self-directed—plays a powerful role in emotional regulation. It’s not about achieving fitness goals or burning calories. It’s about using the body to influence the brain. Research from Harvard Medical School shows that regular physical activity increases the production of endorphins and brain-derived neurotrophic factor (BDNF), a protein that supports neuron growth and resilience in areas linked to mood.
Low-intensity movement is especially effective for those managing depression. A daily 20-minute walk, stretching routine, or gentle yoga session can reduce levels of cortisol, the stress hormone, and lower inflammatory markers associated with depressive symptoms. One study published in JAMA Psychiatry found that even modest physical activity—such as walking three times a week—was linked to a 25% lower risk of developing depression over time. The key isn’t intensity but consistency. Movement becomes a form of self-respect, a quiet act of saying, “I am worth the effort.”
Starting small is crucial. On days when getting out of bed feels like a victory, simply standing by the window and taking five deep breaths counts. The goal is not to push through pain but to reconnect with the body in a non-judgmental way. Some women find rhythm through dancing in the kitchen while making dinner, others through gardening or folding laundry with awareness. These moments build a sense of agency, reminding the nervous system that safety and movement are possible.
Over time, these small acts accumulate. The body begins to expect movement, and the brain responds with greater stability. There will still be heavy days—this is not a cure—but the gap between them may shorten. Movement doesn’t have to be structured or scheduled. It just has to be kind. When approached as a form of care rather than obligation, it becomes a sustainable part of emotional maintenance.
Rhythm of Recovery: The Role of Sleep and Daily Structure
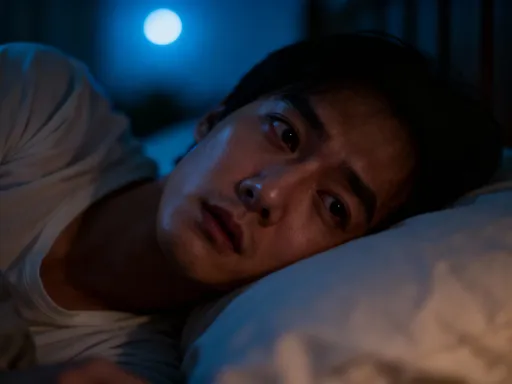
Sleep and mood are deeply intertwined. Disrupted sleep doesn’t just result from depression—it can also worsen it. Many women report lying awake at 3 a.m., mind racing with unanswerable questions, only to feel emotionally raw the next day. This isn’t just fatigue; it’s a neurological consequence of circadian misalignment. The body’s internal clock, regulated by light, temperature, and routine, governs the release of melatonin and cortisol. When this rhythm is disturbed, emotional regulation suffers.
Establishing a consistent wake time—even on weekends—helps anchor the circadian system. Exposure to natural light within 30 minutes of waking signals the brain to stop producing melatonin, the sleep hormone, and begin the day with greater alertness. One effective strategy is having morning tea or coffee near a window or stepping outside for a few minutes, regardless of weather. This simple act strengthens the body’s internal clock, improving both sleep quality and daytime mood.
Evening routines matter just as much. Reducing screen time at least one hour before bed minimizes blue light exposure, which suppresses melatonin. Instead of scrolling, some women find comfort in reading, listening to soft music, or practicing gentle stretches. Creating a buffer between the day’s demands and sleep allows the nervous system to transition from alertness to rest. A warm bath, dim lighting, or a gratitude journal can signal safety to the brain, making it easier to relax.
Structure doesn’t mean rigidity. Life with children, work, or caregiving responsibilities rarely allows for perfect routines. The goal is consistency, not control. On chaotic days, returning to one anchor—like waking at the same time or stepping outside once—can restore balance. Over time, this rhythm becomes a quiet foundation, offering stability even when emotions feel unpredictable. Sleep isn’t a luxury; it’s a cornerstone of emotional resilience.
Fueling Stability: Nutrition’s Subtle Impact on Mood
Food doesn’t cure depression, but what we eat influences how we feel. The brain consumes about 20% of the body’s energy, relying on a steady supply of nutrients to produce neurotransmitters like serotonin and dopamine. Diets high in processed foods, refined sugars, and trans fats have been linked to increased inflammation and a higher risk of depressive symptoms. Conversely, whole-food patterns rich in fiber, omega-3 fatty acids, and antioxidants support brain health and emotional balance.
One study from the SMILES trial demonstrated that participants who followed a Mediterranean-style diet—emphasizing vegetables, fruits, whole grains, legumes, fish, and olive oil—showed significant improvement in depressive symptoms compared to those receiving social support alone. The effects were not immediate, but over 12 weeks, many reported greater clarity, energy, and emotional stability. This doesn’t mean adopting a strict diet; it means making gradual, sustainable shifts.
Simple changes can make a difference. Swapping sugary snacks for nuts or fruit helps stabilize blood sugar, reducing mood swings. Including a source of protein at each meal supports neurotransmitter production. Fatty fish like salmon or sardines provide omega-3s, which are linked to reduced inflammation and improved neural communication. For those who don’t eat fish, flaxseeds, chia seeds, and walnuts offer plant-based alternatives.
Nutrition isn’t about perfection. It’s about patterns. On difficult days, eating may feel like another burden. The goal isn’t to eat perfectly but to nourish the body enough to support healing. Keeping easy options on hand—like hard-boiled eggs, yogurt, or pre-cut vegetables—reduces decision fatigue. Cooking with a child or listening to a podcast while preparing food can turn meals into moments of connection rather than chores. Food, in this way, becomes another form of self-care, quiet and steady.
Connection as Medicine: Why Relationships Matter in Healing
Isolation often feels like the safest place during depression. Reaching out takes energy, and the fear of being misunderstood or judged can be overwhelming. Yet human connection remains one of the most powerful tools for emotional recovery. Social support doesn’t erase pain, but it disrupts the belief that you are alone. Simply saying, “I’m not okay,” to a trusted friend can lighten the weight, even if nothing changes immediately.
Research consistently shows that strong social ties are linked to lower rates of depression and faster recovery. Support doesn’t have to come from deep conversations. Sometimes, sitting quietly with a friend, walking side by side, or sharing a meal provides enough connection to shift the nervous system from survival mode to safety. Support groups, whether in person or online, offer a space where experiences are validated, reducing shame and isolation.
Therapy provides another form of connection—one built on listening without judgment. A trained therapist doesn’t offer solutions but helps uncover patterns, offering tools to navigate difficult emotions. Cognitive behavioral therapy, interpersonal therapy, and mindfulness-based approaches have all shown effectiveness in managing depression. Medication, when appropriate, can be combined with therapy for greater impact. The choice to seek help is not a sign of weakness but an act of courage.
For women who care for others—children, aging parents, partners—asking for support can feel selfish. But emotional health isn’t a luxury; it’s a necessity. When you care for yourself, you preserve your ability to care for others. Connection doesn’t require grand gestures. It begins with small acts of honesty—a text, a phone call, a moment of presence. Over time, these moments build a web of support, reminding you that you are not meant to carry everything alone.
Prevention, Not Perfection: Building a Personal Maintenance Plan
Recovery from depression isn’t a finish line. It’s an ongoing process of adjustment, awareness, and self-compassion. The goal isn’t to eliminate difficult emotions but to build resilience so they don’t consume you. A personal maintenance plan isn’t rigid; it’s flexible, evolving with your needs. It combines the strategies that work for you—movement, sleep, nutrition, connection—into a sustainable rhythm.
Start by identifying your early warning signs. Do you sleep more? Withdraw from conversations? Notice changes in appetite? Write them down. Next, list small actions that help—calling a friend, stepping outside, writing in a journal. Keep this list visible. On hard days, you won’t have to think—just act. Prevention means responding early, before the fog thickens.
Include professional support as part of your plan. Just as you see a doctor for physical health, mental health care is preventive. Regular check-ins with a therapist, even when feeling stable, help maintain emotional balance. If medication is part of your journey, taking it consistently is an act of self-respect, not dependence.
Most importantly, practice self-compassion. There will be setbacks. Some days, getting out of bed is the only victory. That’s enough. Healing isn’t linear. It’s messy, quiet, and deeply personal. By treating yourself with the same kindness you’d offer a friend, you create space for growth. Depression may always be part of your story, but it doesn’t have to define it. You are learning to dance with the heavy days—not to defeat them, but to move through them, one honest step at a time.