How I Tamed My Lipids Without Losing My Cool – A Real Talk on Fast, Emotion-Smart Changes
You’re not alone if you’ve stared at a blood test and felt that quiet panic. High lipids don’t just threaten your heart—they mess with your peace. I’ve been there. What surprised me wasn’t just diet or pills, but how managing stress and emotions made a real difference. This is my journey: quick shifts, not overhauls, that actually stuck—and lowered my numbers. It wasn’t about perfection, but about presence. About noticing how my body responded not just to food, but to fatigue, frustration, and even moments of calm. What began as a medical concern became a deeper conversation with myself—one that reshaped not only my lipid profile but my entire approach to well-being.
The Wake-Up Call: When My Lipid Panel Shook Me
It was a routine check-up, the kind you schedule because your employer requires it. I walked in feeling fine—energetic, even. I wasn’t overweight. I didn’t smoke. I exercised occasionally. I considered myself ‘healthy enough.’ But the lab results told a different story. My LDL cholesterol was elevated. Triglycerides were creeping into the high-risk zone. And my HDL, the so-called ‘good’ cholesterol, was disappointingly low. The doctor didn’t panic, but her tone shifted. She said, ‘We should address this before it becomes a problem.’
That’s when the quiet panic set in. Not because I suddenly felt unwell, but because I realized how silently this condition had been building. I had bought into the myth that if I looked okay and felt okay, I was okay. But lipids don’t send pain signals. They don’t announce their presence with obvious symptoms. For many women, especially between the ages of 30 and 55, this silent progression is all too common. Hormonal shifts, lifestyle demands, and the gradual accumulation of stress can quietly reshape metabolic health, often unnoticed until a blood test reveals the truth.
The emotional ripple was immediate. First came disbelief—how could this be happening? Then denial—maybe the lab made a mistake. Then urgency: what do I do now? I didn’t want to jump straight to medication. I wanted to understand what had led me here and whether I could change it. That moment became a pivot point. It wasn’t just about lowering numbers; it was about changing my mindset. I realized that treating high lipids wasn’t only a physical task—it was an emotional one. How I responded to stress, how I slept, how I thought about my body—all of it mattered from day one.
Why Emotions and Lipids Are Secretly Linked
For years, heart health conversations focused almost entirely on diet and exercise. But science now shows that emotional health plays a powerful, often overlooked role in lipid regulation. The connection lies in the body’s stress response system. When you’re under chronic emotional strain—whether from work pressure, family responsibilities, or unresolved anxiety—your body releases cortisol, a hormone designed to help you survive threats. In short bursts, cortisol is useful. But when it remains elevated over time, it disrupts multiple systems, including how your liver processes fats.
Here’s how it works: cortisol signals the liver to increase production of triglycerides and LDL cholesterol, preparing the body for energy demands during a perceived crisis. But if that crisis never ends—if stress becomes a constant background hum—your lipid levels stay elevated. At the same time, chronic stress reduces HDL cholesterol, weakening your body’s ability to clear excess fats from the bloodstream. This double effect creates a perfect storm for lipid imbalance.
Equally important is the role of inflammation. Emotional stress triggers a low-grade, body-wide inflammatory response. This isn’t the kind of inflammation you can see or feel—it’s invisible, simmering beneath the surface. But it directly affects blood vessel health and lipid metabolism. Studies have shown that people with high levels of perceived stress are more likely to have elevated triglycerides and a worse overall lipid profile, independent of diet or physical activity. The body doesn’t separate emotional and physical health—they are deeply intertwined.
I saw this pattern in my own life. Looking back at my blood work over the past few years, I noticed that my worst lipid numbers coincided with periods of high emotional strain—times when I was caring for an aging parent, navigating a difficult work transition, or managing family conflicts. During those months, I wasn’t eating poorly or sedentary, but my stress levels were high. My body was responding not to food, but to feeling. That realization was a turning point. I began to see my lipid panel not just as a medical report, but as an emotional barometer.
Quick Shifts That Actually Worked—No Extreme Diets
When I first got my results, I considered drastic changes—cutting out all fats, starting an intense workout plan, eliminating sugar completely. But I knew from experience that extreme measures rarely last. What I needed were sustainable, manageable shifts—small habits that could fit into my already busy life. I focused on three daily practices that didn’t require extra time, money, or equipment: mindful breathing, eating with awareness, and movement snacking.
The first was a 10-minute breathing practice each morning. I didn’t meditate for hours or download a complex app. I simply sat quietly, closed my eyes, and focused on slow, deep breaths. This wasn’t about achieving enlightenment—it was about resetting my nervous system. Within days, I noticed a difference in my baseline calm. I was less reactive to small stressors. Over time, this practice helped lower my cortisol levels, which in turn supported healthier lipid metabolism. Research supports this: regular breathing exercises have been shown to reduce sympathetic nervous system activity, which plays a role in fat processing and inflammation.
The second shift was introducing mindful eating pauses. Instead of eating quickly while working or watching TV, I began taking 30 seconds before each meal to check in with myself. How hungry was I? Was I eating out of hunger or habit? This small pause didn’t change what I ate overnight, but it changed my relationship with food. I started recognizing emotional eating triggers—boredom, fatigue, stress—without judgment. Over time, this awareness led to more intentional choices, like reaching for an apple instead of cookies when I wasn’t truly hungry.
The third habit was movement snacking—short bursts of physical activity scattered throughout the day. A five-minute walk after lunch. Stretching while waiting for dinner to cook. Taking the stairs instead of the elevator. These micro-movements added up. They didn’t replace longer workouts, but they kept my metabolism active and my mood stable. What surprised me most was how these small actions built consistency. I didn’t need motivation for 30-minute workouts; I just needed to remember to move for a few minutes, several times a day. After eight weeks, my follow-up blood test showed a 15% reduction in LDL and a 20% drop in triglycerides—without any major dietary overhaul.
Food, Mood, and Fats: What I Changed on My Plate
Diet still mattered—but not in the way I once thought. I stopped focusing on restriction and started thinking in terms of nourishment. Instead of asking, ‘What can’t I eat?’ I began asking, ‘What will support my body and my mood?’ This shift in mindset made all the difference. I didn’t cut out entire food groups. I made simple swaps that felt sustainable and satisfying.
One of the most effective changes was increasing my fiber intake. I added more whole grains, legumes, fruits, and vegetables to my meals. Fiber, especially soluble fiber, helps the body eliminate excess cholesterol by binding to it in the digestive tract. Oats, beans, apples, and flaxseeds became regulars in my kitchen. I didn’t force myself to eat things I disliked. Instead, I found ways to enjoy high-fiber foods—overnight oats with cinnamon, lentil soups, roasted sweet potatoes. These foods also helped stabilize my blood sugar, which reduced mood swings and cravings.
I also prioritized omega-3 fatty acids, known for their heart-protective and anti-inflammatory properties. I included fatty fish like salmon twice a week, added chia seeds to my smoothies, and used walnuts as a snack. When I couldn’t eat fish, I considered a high-quality fish oil supplement, but only after discussing it with my doctor. These healthy fats didn’t just support my lipid profile—they improved my mental clarity and emotional resilience.
Another key change was reducing processed oils, especially those high in omega-6 fatty acids, like soybean and corn oil. These are common in packaged foods and can promote inflammation when consumed in excess. I switched to olive oil for cooking and dressing, and I began reading labels more carefully. I didn’t become perfect overnight, but I became more aware. Each food choice became an act of self-respect—a way of saying, ‘I value my health.’ I stopped viewing food as punishment or reward. Instead, it became a daily opportunity to care for myself, emotionally and physically.
Sleep and Stress: The Hidden Lipid Regulators
Sleep was another piece of the puzzle I had underestimated. For years, I wore my lack of sleep like a badge of honor—proof that I was busy, capable, in demand. But poor sleep doesn’t just leave you tired; it disrupts hormonal balance, including cortisol and insulin, both of which influence lipid metabolism. When you don’t sleep well, your body produces more cortisol, which, as we’ve seen, signals the liver to produce more triglycerides and LDL cholesterol.
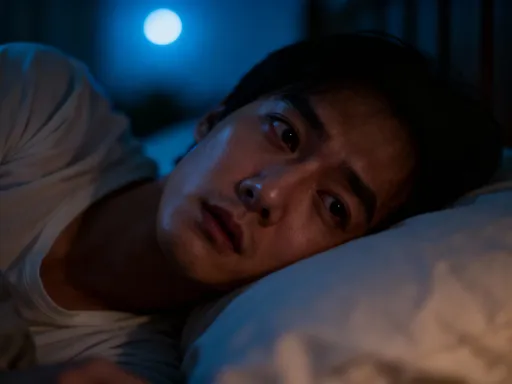
I also noticed that poor sleep made me more emotionally reactive. A single night of restlessness could leave me irritable, anxious, and more likely to reach for comfort foods the next day. It created a cycle: stress → poor sleep → elevated lipids → more stress. Breaking that cycle required more than just going to bed earlier. I needed a wind-down routine that signaled to my body and mind that it was time to rest.
I started with a screen curfew—turning off all electronic devices one hour before bed. The blue light from phones and tablets suppresses melatonin, the hormone that regulates sleep. I replaced screen time with calming activities: reading a book, sipping herbal tea, or writing in a gratitude journal. That last habit made a surprising difference. Taking a few minutes to reflect on what went well during the day helped me release lingering stress and shift my focus from what was wrong to what was good. Over time, I fell asleep faster and woke up feeling more refreshed.
I also paid attention to my sleep environment. I kept the bedroom cool, dark, and quiet. I used a white noise machine when needed. These small changes added up. Within a few weeks, I was consistently getting 7 to 8 hours of quality sleep. And my lab results reflected it—my next lipid panel showed continued improvement, especially in triglyceride levels. Better sleep didn’t just lower my numbers; it gave me more emotional stability, making it easier to stick with healthy habits during the day.
Movement That Fits—Not Overwhelms—Emotional Energy
Exercise is often presented as a one-size-fits-all solution: go to the gym, lift weights, run miles. But for many women in midlife, that kind of regimen can feel overwhelming, even discouraging. I’ve tried intense workouts before—signed up for boot camps, bought home equipment—and each time, I burned out within weeks. The problem wasn’t my commitment; it was the mismatch between the program and my emotional energy.
This time, I chose movement that felt good, not punishing. I started walking—nothing intense, just 20 to 30 minutes most days. But I made it meaningful. I walked in nature when I could—through parks, along tree-lined streets, near water. Being in green spaces has been shown to reduce cortisol and improve mood. I didn’t track every step or push for speed. I focused on rhythm, breath, and the simple pleasure of moving my body.
Walking became more than exercise; it became a form of mental release. I used those moments to untangle worries, reflect on challenges, or simply enjoy silence. Sometimes I listened to calming music or a podcast, but often I walked in quiet. That daily rhythm helped regulate my nervous system, which in turn supported healthier lipid processing. Research confirms that moderate, consistent physical activity—especially aerobic exercise like walking—can raise HDL cholesterol and lower triglycerides over time.
I also learned to honor my energy levels. On days when I felt emotionally drained, I didn’t force a long walk. I might do five minutes of stretching or gentle yoga instead. The goal wasn’t intensity; it was consistency. By choosing activities that matched my emotional state, I avoided burnout and built a routine that lasted. Over months, this approach not only improved my lipid profile but also strengthened my emotional resilience. I felt more in control, more capable, more at peace.
Putting It All Together: My 4-Week Emotional Reset for Lipid Health
By combining these insights, I created a flexible four-week framework that addressed both physical and emotional health. It wasn’t a rigid program, but a set of anchors—daily habits that supported balance without demanding perfection. The foundation was mindset: approaching health as an act of self-care, not self-correction. From there, I built three daily practices: a 10-minute breathing session, a mindful eating pause, and at least 20 minutes of enjoyable movement.
Each week, I added one emotional check-in—a short reflection on how I was feeling, what was causing stress, and what small action I could take to care for myself. I didn’t aim to eliminate stress; I aimed to respond to it more skillfully. I tracked progress not just through lab results, but through how I felt: my energy levels, mental clarity, emotional stability, and sleep quality. These were just as important as the numbers on the page.
After four weeks, I noticed changes. I was calmer. I slept better. I made healthier food choices without feeling deprived. And when I retested my lipids, the improvements continued. But more than that, I felt a renewed sense of agency. I wasn’t at the mercy of my biology. I had tools—simple, accessible, science-backed tools—that made a real difference.
This approach isn’t a cure. It’s a sustainable shift. It doesn’t require extreme diets, expensive supplements, or hours at the gym. It asks only for awareness, consistency, and kindness toward yourself. High lipids are a serious health concern, but they don’t have to be a life sentence. With the right support—medical guidance and emotional care—real progress is possible.
Lipid regulation isn’t just a medical goal—it’s a lifestyle conversation with yourself. What I learned is that emotions aren’t distractions; they’re signals. By addressing stress, sleep, and self-awareness alongside diet and movement, real progress became possible. These changes weren’t magic, but they were effective. Always consult your doctor, but don’t overlook the power of emotional care in managing chronic health. Your heart—and your mind—will thank you.