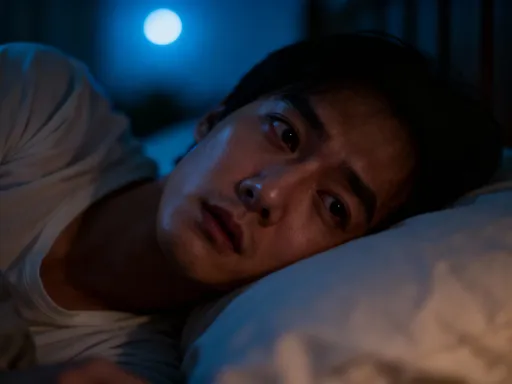
You’re Not Tired—Your Mind Just Can’t Shut Off
Ever lie in bed, physically exhausted but mentally wide awake? You’re not alone. Millions struggle with restless minds that sabotage sleep, even when the body craves rest. This isn’t just about feeling groggy—it’s about how psychological patterns silently disrupt recovery. In this article, we’ll explore the invisible mental barriers to deep, restorative sleep and break down a systematic approach to reset your mind, reclaim calm, and finally get the quality rest you truly need. While fatigue may weigh on the body, an overactive mind refuses to surrender, creating a nightly battle between exhaustion and endless thought. The good news is that this cycle can be broken—not with pills or drastic changes, but through understanding and gently retraining the mind.
The Hidden Problem: Why “Being Tired” Doesn’t Guarantee Sleep
Physical exhaustion does not automatically lead to sleep. Many women in their 30s, 40s, and 50s experience this disconnect nightly: aching limbs, heavy eyes, and a schedule that demands rest—yet the mind races with unresolved thoughts, tomorrow’s to-do lists, or replayed conversations. This mismatch between body and brain is more common than many realize, and it lies at the heart of what sleep specialists call cognitive insomnia. Unlike insomnia caused by medical conditions or medications, cognitive insomnia stems from mental hyperarousal—a state where the brain remains alert despite physical fatigue.
The human brain evolved to prioritize survival, not rest. When it senses unresolved issues—emotional tensions, unmet responsibilities, or even subconscious anxieties—it resists shutdown. For many, this mental vigilance has become habitual. The brain interprets stillness as risk, and silence as a signal to scan for threats. In modern life, these threats are rarely physical; they are psychological—work pressures, family obligations, financial concerns. Yet the brain responds the same way, flooding the system with low-grade stress hormones like cortisol, which interfere with the natural sleep onset process.
Chronic stress plays a major role in sustaining this cycle. When stress becomes a background hum rather than an occasional spike, the nervous system adapts to a state of constant readiness. This is known as sympathetic dominance—the body’s “fight or flight” mode. Over time, the brain begins to associate bedtime not with safety, but with an opportunity to finally process the day’s unresolved emotions and thoughts. The result is a paradox: the more tired a person becomes, the more their mind activates during the transition to sleep.
Modern lifestyles amplify this problem. Constant connectivity, multitasking, and the cultural glorification of busyness have normalized mental overactivity. Many women report feeling guilty for resting, as if downtime is wasted time. This belief, often subconscious, reinforces the idea that the mind must always be productive. When sleep becomes another task to “get right,” the pressure intensifies, further blocking the very state being sought. Traditional sleep advice—such as maintaining a consistent bedtime or avoiding caffeine—often fails because it addresses the physical environment while ignoring the internal mental climate.
Rewiring the Brain: How Psychological Patterns Control Sleep Readiness
Sleep is not merely the absence of wakefulness; it is an active psychological surrender. The brain must transition from a state of engagement to one of disengagement, from doing to being. This shift depends on a delicate balance between the sympathetic nervous system, which keeps us alert, and the parasympathetic nervous system, which promotes relaxation and recovery. When this balance is disrupted by persistent mental activity, sleep readiness diminishes, even in the presence of fatigue.
Habitual thought patterns play a critical role in this process. The brain operates on neural pathways shaped by repetition. When someone routinely engages in late-night rumination—replaying conflicts, worrying about the future, or analyzing past decisions—these circuits become stronger and more automatic. Over time, the brain learns to expect and even default to this mental activity at bedtime. What begins as a response to stress becomes a conditioned behavior, like muscle memory for the mind.
Emotional triggers also contribute to sleep resistance. For example, a woman who feels overwhelmed by caregiving responsibilities may find that as soon as she lies down, thoughts about her children, aging parents, or household duties flood in. These thoughts are not random; they are tied to deeply held values and roles. The brain interprets these concerns as urgent, even if they cannot be resolved at that moment. This creates a sense of psychological urgency that overrides physical tiredness.
Subconscious beliefs about productivity further complicate the issue. Many women internalize the message that worth is tied to output—that rest is only earned after all tasks are complete. This mindset makes it difficult to grant oneself permission to stop. The mind remains in a state of “on-call” readiness, scanning for unfinished business. In this context, sleep is not seen as a biological necessity, but as a luxury that must be justified. When rest feels undeserved, the brain resists it, maintaining a low level of mental alertness as a form of self-policing.
Neuroscience confirms that repeated mental habits reshape brain function. Functional imaging studies show that individuals with chronic sleep onset difficulties exhibit heightened activity in the prefrontal cortex—the region responsible for planning, decision-making, and self-regulation—during the transition to sleep. This suggests that their brains are still in problem-solving mode when they should be winding down. The good news is that neuroplasticity allows for change. With consistent practice, new pathways can be formed, and the brain can be retrained to associate bedtime with safety, release, and calm.
The Pre-Sleep Mindset: Building a Mental Routine for Rest
Just as a bedtime routine signals the body that it’s time to sleep, a mental routine can signal the brain. The goal is not to eliminate thoughts—this is neither possible nor necessary—but to create a structured way of managing them so they don’t dominate the night. A pre-sleep mindset is about psychological preparation, helping the mind transition from engagement to surrender without resistance.
One effective strategy is scheduling a designated “worry time” earlier in the evening. This involves setting aside 15 to 20 minutes—ideally two hours before bed—to consciously review concerns, make notes, or plan solutions. By containing worry to a specific window, the brain learns that it does not need to process these thoughts at bedtime. This technique leverages the brain’s preference for closure. When a person knows they have already addressed their concerns, the mind is more likely to let go of them when it’s time to rest.
Cognitive defusion, a concept from acceptance and commitment therapy, is another powerful tool. It involves observing thoughts without attaching to them or treating them as facts. For example, instead of thinking, I’ll never get to sleep, a person might reframe it as, I’m having the thought that I’ll never get to sleep. This subtle shift creates distance, reducing the emotional weight of the thought. Over time, this practice weakens the grip of repetitive, sleep-disrupting narratives.
Mental containment techniques, such as the “worry box” visualization, can also be helpful. This involves imagining a box where one places troubling thoughts before bed. The person mentally writes down their worries, puts them in the box, and closes the lid, symbolizing that these issues are safely stored and can be revisited tomorrow. This ritual provides psychological closure, satisfying the brain’s need for order and control without requiring actual problem-solving.
Consistency is more important than intensity. These practices do not need to be perfect or deeply elaborate to be effective. What matters is regularity. Over weeks and months, small shifts in thinking accumulate, gradually reshaping the brain’s expectations around bedtime. The mind begins to associate the evening not with unresolved tension, but with a predictable sequence of release and transition. This sense of predictability enhances psychological safety, making it easier to let go.
Breathing, Body, and Belief: Integrating Physical and Mental Calm
The mind and body are deeply interconnected, especially when it comes to sleep. While mental habits influence physical states, the reverse is also true: physical actions can signal psychological safety. When the body relaxes, the brain receives feedback that it is safe to disengage. This bidirectional relationship makes physical relaxation techniques essential tools for improving sleep readiness.
Controlled breathing is one of the most accessible and effective methods. Slow, rhythmic breathing activates the vagus nerve, a key component of the parasympathetic nervous system. This sends a direct signal to the brain that the body is not under threat. A simple technique is paced respiration: inhaling slowly through the nose for a count of four, holding for a count of two, and exhaling gently through the mouth for a count of six. Repeating this cycle for five to ten minutes lowers heart rate, reduces muscle tension, and calms mental chatter.
Body scanning is another powerful practice. It involves mentally moving attention through different parts of the body, starting from the toes and moving upward. As each area is noticed, the person consciously releases any tension they may be holding. This practice combines mindfulness with physical relaxation, grounding the mind in the present moment. Because rumination often involves future-oriented or past-focused thinking, body scanning anchors awareness in the now, interrupting the cycle of mental wandering.
Progressive muscle relaxation (PMR) takes this a step further by actively tensing and then releasing muscle groups. For example, a person might tighten their foot muscles for five seconds, then release and notice the difference in sensation. This process is repeated through the legs, abdomen, arms, and face. PMR works by increasing awareness of physical tension and teaching the body what true relaxation feels like. Over time, the contrast between tension and release becomes more noticeable, making it easier to recognize and let go of stress before it builds.
These techniques are most effective when practiced regularly, not just at bedtime. Daily use strengthens the mind-body connection, making it easier to access calm when needed. They also help break the cycle of mental vigilance—where the brain constantly scans for threats—by replacing it with a pattern of intentional release. When the body learns to relax on cue, the mind follows, creating a smoother transition into sleep.
Digital Detox and Mental Clutter: Managing Cognitive Load Before Bed
In today’s world, one of the greatest barriers to mental shutdown is digital overstimulation. Screens are not only sources of blue light, which suppresses melatonin, but also gateways to endless cognitive input. Each notification, email, or social media update triggers a micro-surge of attention, keeping the brain in a state of alertness. For many women, the evening routine includes scrolling through news, checking messages, or watching videos—activities that increase, rather than reduce, mental load.
The psychological pull of digital devices is strong. They offer instant gratification, distraction from discomfort, and a sense of connection. But this comes at a cost. The brain does not distinguish between important and trivial information when it comes to processing load. Whether reading a work email or watching a lighthearted video, the mind is still engaged in decoding, interpreting, and storing information. This cognitive activity delays the natural wind-down process, making it harder to transition into rest.
Information overload is particularly disruptive because it prevents mental closure. When the brain is bombarded with new content late into the evening, it lacks the time to process and file away the day’s experiences. This leads to a sense of mental clutter—a feeling of being mentally “full” without resolution. As a result, the mind remains active, trying to make sense of fragmented inputs long after the screen is off.
A structured evening protocol can help reduce this burden. This begins with setting a digital curfew—at least one hour before bedtime—during which screens are minimized or avoided altogether. Instead, this time can be dedicated to low-stimulus activities such as reading a physical book, journaling, light stretching, or listening to calming music. These activities support mental decompression without adding cognitive strain.
Equally important is creating psychological boundaries around technology use. This means not only turning off devices but also mentally disengaging from their content. For example, if a person checks work emails in the evening, they may continue to think about those messages even after logging off. A better approach is to designate specific times for digital engagement and stick to them, allowing the mind to expect and accept periods of disconnection. Over time, this builds a healthier relationship with technology, reducing its power to disrupt rest.
The Long Game: Tracking Progress and Adjusting the System
Improving sleep through mental retraining is not a linear process. There will be nights of progress and nights of setback. This is normal. The key is not perfection, but awareness and adaptation. Tracking subtle changes—such as falling asleep faster, waking up fewer times, or feeling more refreshed in the morning—provides valuable feedback on what is working and what may need adjustment.
Non-judgmental self-observation is essential. Instead of labeling a restless night as a failure, it can be viewed as data. For example, if a woman notices she sleeps better on nights when she practices breathing exercises but worse when she watches intense TV shows, she gains insight into her personal sleep triggers. This kind of awareness empowers her to make informed choices without self-criticism.
Journaling can support this process. A simple sleep log that records bedtime, wake time, perceived sleep quality, and evening activities can reveal patterns over time. It may show, for instance, that consuming news before bed consistently leads to delayed sleep onset, or that a consistent wind-down routine improves morning alertness. These insights allow for gradual refinement of the sleep system.
Flexibility is also important. What works for one person may not work for another, and needs may change over time. A technique that feels helpful initially—such as a worry journal—may lose effectiveness after a few weeks. This is not a sign of failure, but an invitation to explore other tools. The goal is sustainable integration, not rigid adherence to a single method. By staying curious and patient, women can develop a personalized approach that evolves with their lives.
Sleep as a Practice: Reclaiming Rest Without Pressure
True rest is not something that can be forced. The harder one tries to fall asleep, the more elusive it becomes. This paradox lies at the heart of many sleep struggles. When sleep is treated as a performance—something to achieve or measure—it becomes another source of pressure. The solution is not to try harder, but to let go.
Sleep is best approached as a practice, like breathing or walking—something natural that unfolds when conditions are right. This shift in perspective reduces outcome dependency. Instead of focusing on getting to sleep, the emphasis moves to creating the conditions for sleep. This includes cultivating psychological safety, practicing self-compassion, and releasing the need to control the process.
Self-compassion is especially important. Many women carry guilt or frustration when they can’t sleep, as if it reflects a personal failing. But sleep is not a moral issue. It is a biological rhythm influenced by countless factors, many of which are beyond direct control. Treating oneself with kindness—acknowledging effort, accepting imperfection, and recognizing progress—creates an internal environment where rest can flourish.
Detachment from outcome pressure is equally vital. This means lying down not to make sleep happen, but to invite it. It means allowing thoughts to come and go without engaging them, trusting that rest will come in its own time. This trust is built through consistent practice and repeated positive experiences. Over time, the mind learns that rest is not a reward for productivity, but a fundamental right—a necessary part of being human.
By reframing sleep as a rhythm rather than a task, women can finally stop chasing it. They can stop analyzing, monitoring, and striving. Instead, they can return to a simpler truth: the body knows how to rest. The mind only needs to stop getting in the way.